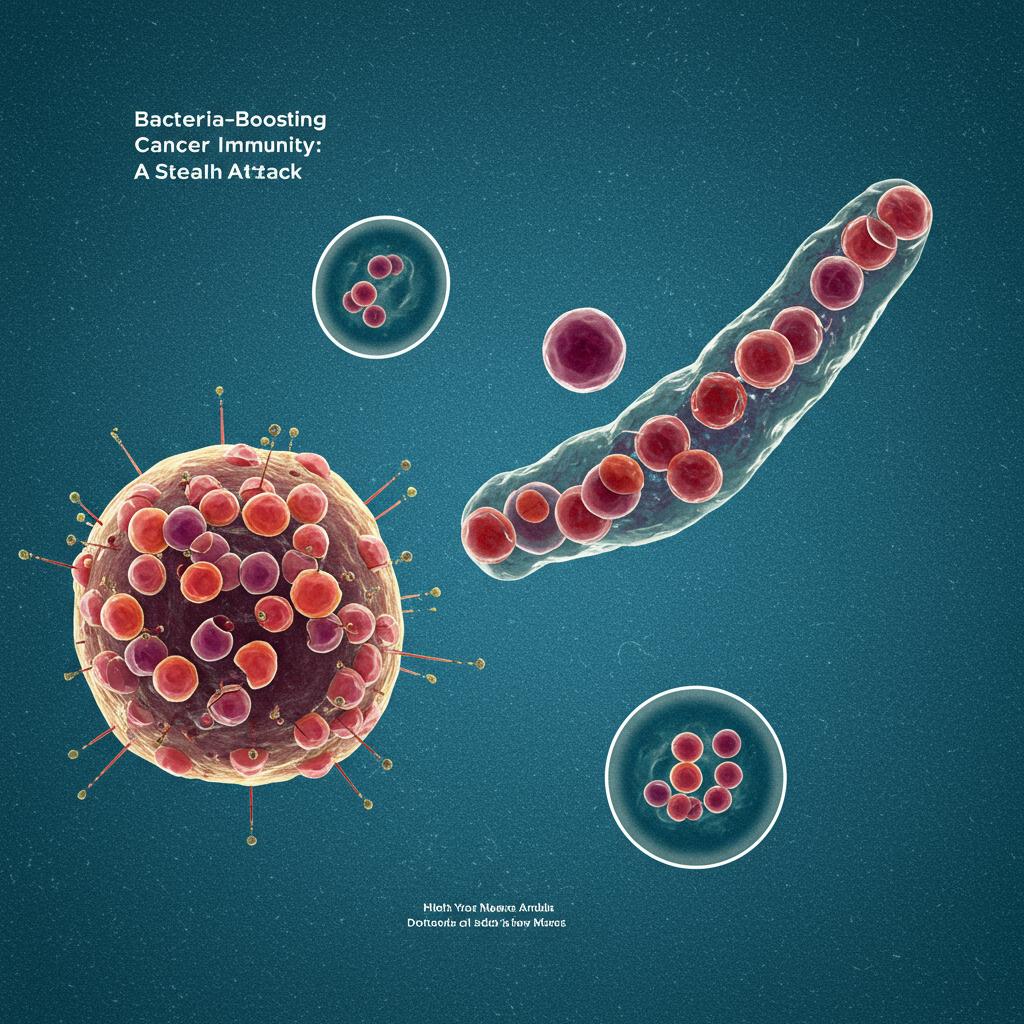
Ever heard of using bacteria to fight cancer? It sounds a bit wild, right? But bacterial immunotherapy is a rapidly evolving field with some seriously exciting potential. It’s all about harnessing the power of certain bacteria to boost our own immune system’s ability to attack and destroy tumors. However, it’s not as simple as just injecting bacteria and watching the magic happen. There’s a complex interplay happening within the tumor, and understanding this is key to unlocking the full potential of this promising therapy.
Our research focused on a specifically engineered strain of Salmonella enterica, a bacteria known for its ability to both survive within tumors and activate the immune system. We discovered a fascinating mechanism that explains how this bacteria manages to perform this seemingly contradictory dual role. It all comes down to a receptor called IL-10R, which is found on immune cells.
Here’s the breakdown:
- The IL-10R “switch”: Think of IL-10R as a kind of switch on immune cells. Inside tumors, this switch gets flipped into a high-expression state (IL-10Rhi). This change isn’t just a minor tweak; it fundamentally alters how these immune cells behave.
- Helping the helpers and hindering the hunters: Our engineered Salmonella takes advantage of this flipped switch. It encourages tumor-associated macrophages, a type of immune cell, to produce IL-10, a molecule that dampens the immune response. This might seem counterintuitive, but it’s a crucial step. By increasing IL-10, the bacteria essentially creates a shield, protecting itself from attack by other immune cells, like tumor-associated neutrophils, whose job is to gobble up invaders. This allows the bacteria to survive within the tumor environment.
- Waking up the exhausted soldiers: Simultaneously, this increase in IL-10, combined with the presence of the bacteria, has a completely different effect on another type of immune cell: CD8+ T cells. These are the heavy hitters of the immune system, the cells specifically trained to kill cancerous cells. However, within the tumor, these T cells often become exhausted and ineffective. The unique environment created by the bacteria and the increased IL-10 actually revitalizes these exhausted CD8+ T cells, boosting their numbers and stimulating them to attack the tumor.
The result? A powerful combination that effectively eliminates tumors, prevents them from coming back, and even stops them from spreading to other parts of the body. We’ve seen this effect across multiple types of tumors in our preclinical models.
What’s even more exciting is that our analysis of human tumor samples suggests that this IL-10Rhi state – the flipped switch – might be a common feature across many human cancers. This opens up the possibility that this bacterial immunotherapy approach could have broad applications in treating a variety of cancers.
This research gives us valuable insight into how bacterial immunotherapy works against solid tumors and offers a new framework for manipulating the immune response within the tumor environment. While more research is needed, these findings represent a significant step forward in the fight against cancer. We’re hopeful that this approach can one day be translated into effective therapies that bring new hope to patients.
