Understanding the variability in how Alzheimer’s disease affects individuals is crucial for developing effective treatments and support strategies. Currently, the available biomarkers, which measure proteins like amyloid-beta and tau in the brain, don’t fully explain the wide range of cognitive decline observed in Alzheimer’s patients. They only account for about 20-40% of the differences in cognitive impairment. This means there are other factors at play that we need to understand.
Think of it like this: if you were trying to predict how fast a car would go, knowing the engine size would give you some information, but not the whole picture. You’d also need to consider factors like tire pressure, wind resistance, and the driver’s skill. Similarly, with Alzheimer’s, we need to find additional “factors” besides amyloid-beta and tau to better understand cognitive decline.
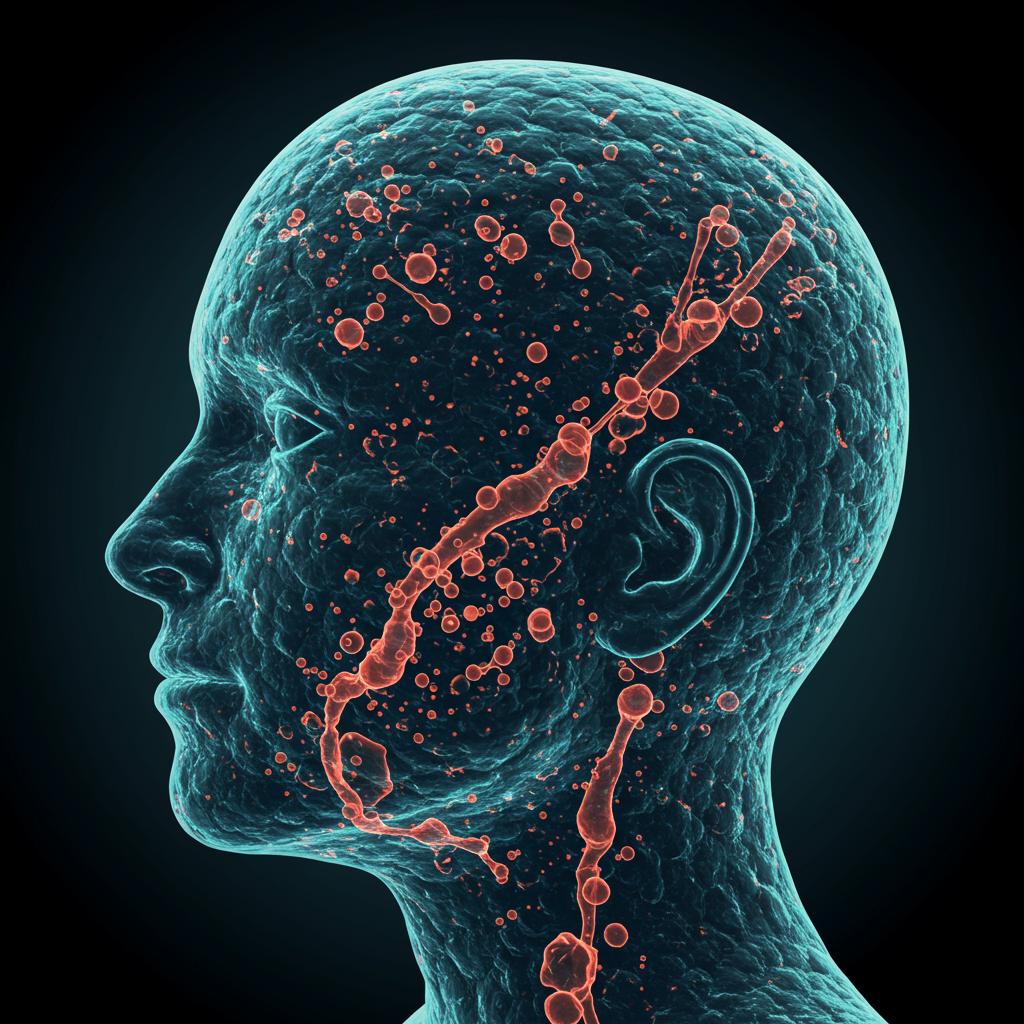
In a large-scale study involving thousands of individuals, researchers examined cerebrospinal fluid (CSF) – the fluid that surrounds the brain and spinal cord – looking for additional clues. They analyzed the proteins within the CSF and discovered that proteins related to synapses, the connections between brain cells, were strongly linked to cognitive impairment. These synaptic proteins offered insights beyond what amyloid-beta and tau could tell us.
Here’s a breakdown of the key findings:
- Synapse Proteins and Cognitive Impairment: The research identified a strong correlation between synapse proteins and the degree of cognitive impairment in individuals with Alzheimer’s, even after accounting for amyloid-beta and tau levels. This points to synapse dysfunction as a significant driver of cognitive issues in Alzheimer’s.
- A New Biomarker Ratio: Scientists developed a ratio using two specific synapse proteins found in CSF: YWHAG and NPTX2 (CSF YWHAG:NPTX2). This ratio proved to be a powerful predictor of cognitive decline, outperforming existing biomarkers in explaining the variance in cognitive impairment.
- Predicting Future Decline: Impressively, the CSF YWHAG:NPTX2 ratio could also predict the likelihood of someone progressing from mild cognitive impairment to dementia over a 15-year period. This suggests its potential as a prognostic tool for monitoring disease progression.
- Early Detection Potential: The CSF YWHAG:NPTX2 ratio was also elevated in individuals with a genetic predisposition to Alzheimer’s even 20 years before estimated symptom onset. This raises the possibility of using this ratio for early detection and intervention.
- Moving Beyond CSF: Recognizing the challenges of obtaining CSF samples, the researchers also explored blood-based biomarkers. They developed a plasma proteomic signature that partially reflected the CSF YWHAG:NPTX2 ratio, offering a less invasive method for assessing cognitive decline in the future.
This research provides a significant step forward in our understanding of Alzheimer’s disease. By focusing on synapse dysfunction and developing new biomarkers like the CSF YWHAG:NPTX2 ratio, we can gain a more complete picture of the disease process and potentially develop more targeted interventions. The possibility of using a blood test to track these changes is particularly exciting, as it could make monitoring and early detection much more accessible. Further research is needed to validate these findings and explore the potential clinical applications of these discoveries, but this work offers a new avenue for hope in the fight against Alzheimer’s.
