Ever heard of microbial amino-acid-conjugated bile acids, or MABAs for short? They’re a relatively new discovery, and scientists are still figuring out exactly what they do in our bodies. One thing’s for sure though: they’re turning out to be pretty important, especially when it comes to type 2 diabetes.
Recent research has uncovered a fascinating link between a specific MABA called tryptophan-conjugated cholic acid (Trp-CA) and type 2 diabetes. It turns out that people with this condition tend to have significantly lower levels of Trp-CA, and the less Trp-CA they have, the worse their blood sugar control tends to be. This suggests that Trp-CA might actually play a role in managing blood sugar levels.
But how does it work? Scientists discovered that Trp-CA interacts with a receptor in our bodies called MRGPRE (Mas-related G protein-coupled receptor family member E). Think of receptors as tiny docking stations on our cells, and Trp-CA is like a key that fits into that specific lock. When Trp-CA binds to MRGPRE, it triggers a cascade of events within the cell that ultimately helps regulate blood sugar.
This interaction happens through two main pathways:
- The MRGPRE-Gs-cyclic AMP (cAMP) pathway: This pathway is like a cellular communication system. When Trp-CA binds to MRGPRE, it activates a protein called Gs, which in turn increases the levels of a messenger molecule called cAMP. This messenger then sets off a chain reaction that leads to improved glucose metabolism.
- The MRGPRE-β-arrestin-1-aldolase A (ALDOA) pathway: This pathway involves another important protein called β-arrestin-1 and an enzyme called aldolase A. When Trp-CA activates MRGPRE, it brings β-arrestin-1 and aldolase A together, which also contributes to the positive effects on blood sugar control.
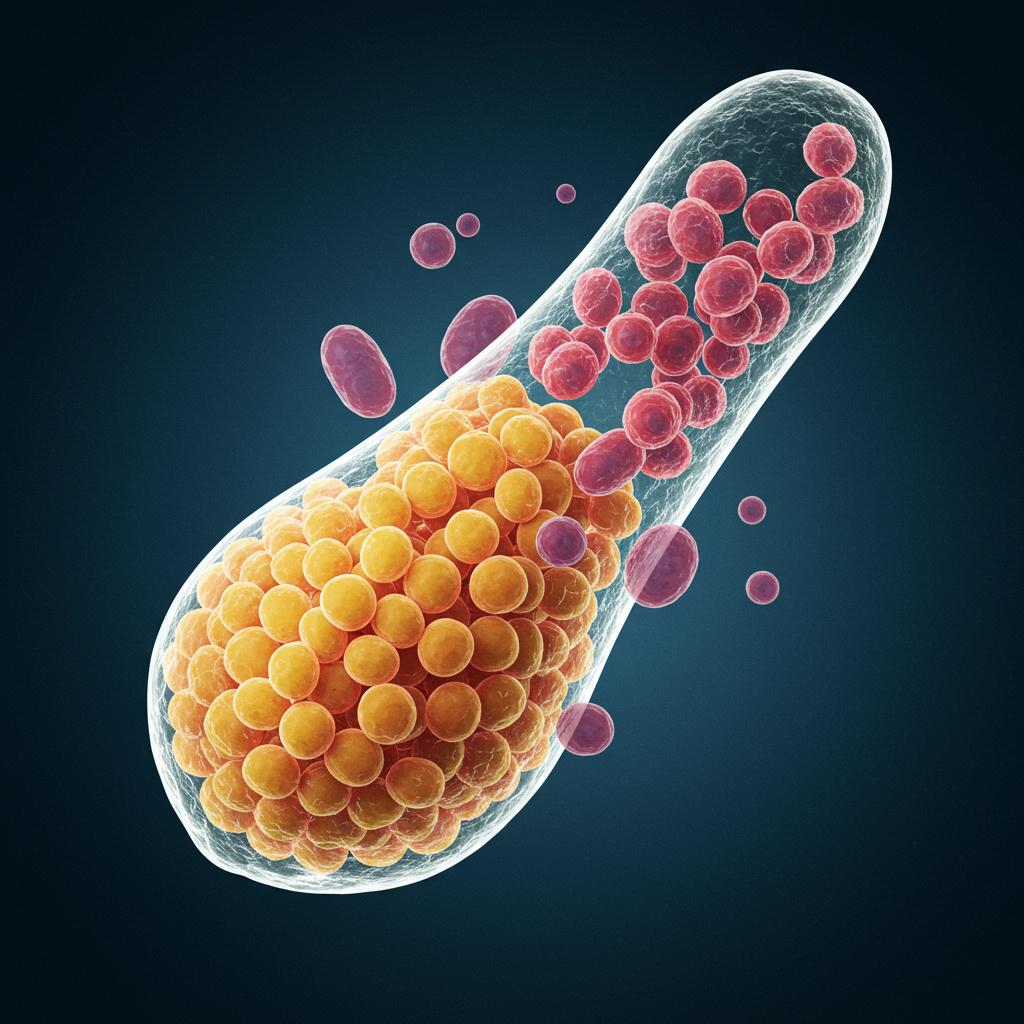
So, where does Trp-CA come from? Interestingly, it’s not something our bodies produce directly. Instead, it’s made by friendly bacteria living in our gut, specifically a type of bacteria called Bifidobacterium. These helpful microbes have an enzyme that can transform bile acids into Trp-CA. This discovery highlights the crucial role of our gut microbiome in our overall health and wellbeing.
This research is exciting for several reasons. First, it sheds light on the importance of MABAs and their potential role in managing type 2 diabetes. It also identifies MRGPRE as a potential new drug target. Imagine a medication designed to mimic the effects of Trp-CA, helping people with diabetes better control their blood sugar.
Finally, this research underscores the importance of a healthy gut microbiome. Supporting the growth of beneficial bacteria like Bifidobacterium through a balanced diet and potentially probiotics could be a crucial step in maintaining healthy blood sugar levels. This study opens up exciting new avenues for research into MABAs, the gut microbiome, and the development of innovative therapies for type 2 diabetes. It’s a reminder of the intricate connections within our bodies and the powerful influence of the tiny microbes that call us home.
