Ever wondered how fungi, those fascinating organisms we usually associate with mushrooms and mold, can sometimes cause infections in humans? It’s a complex process, but let’s break it down into a few key requirements. Think of it as a checklist for fungal invaders:
- Thriving in the Heat: First, they need to be comfortable at our body temperature. Just like we wouldn’t do well in a freezer, fungi that can’t handle our internal warmth are out of luck.
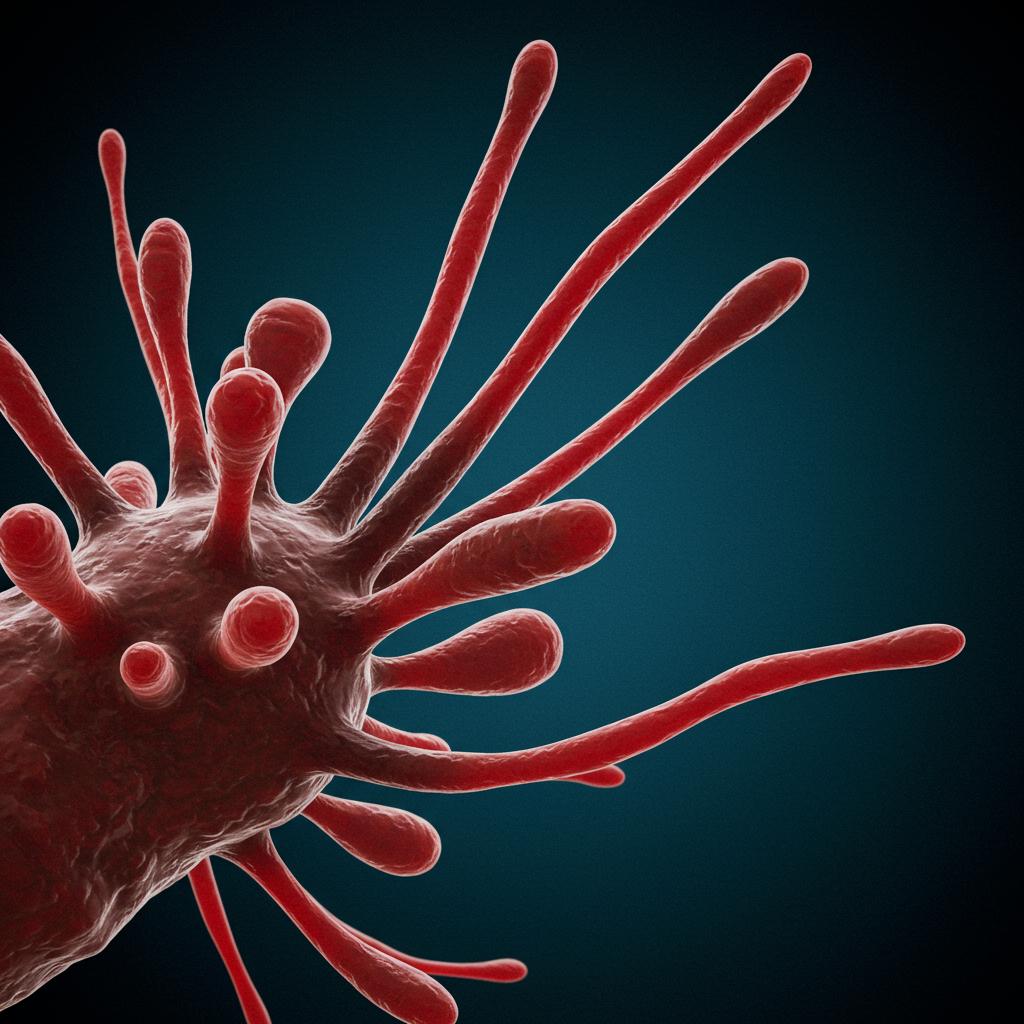
- Breaking and Entering: Next, they need a way to get past our body’s defenses, like skin and mucous membranes. Some fungi are like tiny burglars, sneaking through cracks, while others are more like demolition crews, actively breaking down barriers. They achieve this incredible feat by morphing between small, detachable cells, perfect for spreading, and long, connected cells, ideal for penetrating tissue. This shape-shifting ability is crucial for navigating our bodies.
- Dinner Time: Once inside, they need to eat! They release enzymes that break down our tissues into nutrients they can absorb. It’s a bit like having a microscopic composting operation going on inside you.
- Dodging the Immune System: Finally, they need to evade our immune system, which is constantly patrolling for invaders. This is arguably the most challenging hurdle. Our immune systems are incredibly powerful, and they’ve evolved alongside fungi, developing sophisticated defenses. This constant battle has shaped the evolution of both humans and fungi.
Surprisingly, modern medicine, while life-saving in many ways, can inadvertently make some people more vulnerable to fungal infections. Treatments like chemotherapy and organ transplants can suppress the immune system, giving opportunistic fungi a chance to take hold.
So, how do different types of fungi manage to tick all the boxes on this infection checklist? Well, they each have their own unique strategies. Some fungal groups, like the Entomophthorales, Mucorales, Ascomycota, and Basidiomycota, employ diverse tactics to overcome our defenses.
For example, certain fungi, like Histoplasma and Coccidioides, have a clever trick called thermal dimorphism. They can switch between different forms depending on the temperature, which helps them adapt to different environments, including our bodies. Cryptococcus species can infect both healthy and immunocompromised individuals, highlighting their adaptability. Other fungi, like Candida, Pneumocystis, and Aspergillus, are more likely to cause infections in people with weakened immune systems.
We also shouldn’t forget about the fungi that cause neglected tropical diseases like mycetoma and paracoccidiomycosis. These diseases disproportionately affect people in developing countries and often receive less attention and research funding. Even common fungal infections like athlete’s foot, caused by dermatophytes, can occasionally lead to more serious complications.
The relationship between humans and fungi isn’t always about infection, though. Some fungi live harmlessly on our skin and even play beneficial roles. This peaceful coexistence, known as commensalism, has also influenced the evolution of both fungi and humans.
Understanding how fungi infect humans is crucial for developing effective treatments and preventative strategies. As medical advancements continue and our understanding of fungal pathogens deepens, we can hope for better ways to combat these sometimes-overlooked infections.
