Ever since their arrival on the scene, PD-1 pathway inhibitors have been a game-changer in cancer treatment. But here’s the catch: they don’t work for everyone. A significant number of patients don’t experience lasting benefits, which emphasizes the urgent need for reliable biomarkers. These biomarkers would act like signposts, guiding us to identify patients who are most likely to respond to this type of therapy.
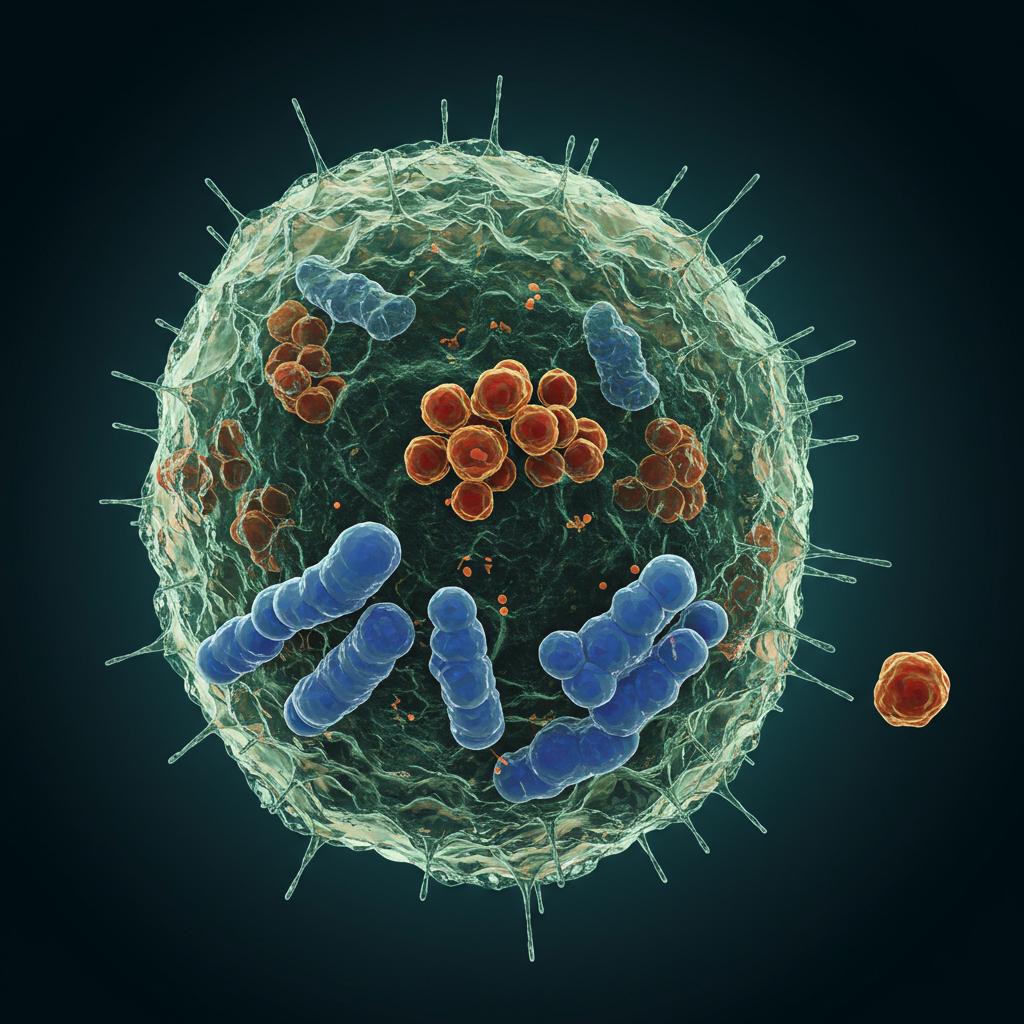
We know that CD8+ tumor-infiltrating lymphocytes (TILs), a type of immune cell that infiltrates the tumor, are linked to a positive response to immune checkpoint therapy. However, there’s a lot of debate about which specific subgroups of these CD8+ TILs are the most valuable predictors of treatment success. Think of it like trying to pick the best player on a basketball team – you need to understand each player’s individual strengths.
Preclinical research has honed in on a group called progenitor-like exhausted CD8+ T cells (TPEX). These cells seem promising because they multiply more actively in response to PD-1 inhibitors compared to other exhausted T cells (TEX). However, it’s not quite that simple. When patients receive immune checkpoint inhibitor (ICI) treatment, these TPEX cells morph into other TEX populations that can also fight the tumor. This cellular transformation makes it tricky to pinpoint precisely which T cell populations are the key players in predicting how a patient will respond to ICI treatment.
Our study delved into this complexity, specifically focusing on advanced melanoma patients. We discovered something interesting: patients with at least 20% of their CD8+ TILs co-expressing both PD-1 and CTLA-4 (we call these CPHi TILs) showed significantly better outcomes after PD-1 monotherapy. They experienced improved objective response rates (meaning the tumor shrank significantly) and longer survival compared to patients below this 20% threshold.
To understand what makes these CPHi TILs so special, we used both bulk and single-cell RNA sequencing to analyze their characteristics. While we did find TPEX-like cells within the CPHi group, they were surprisingly outnumbered by other cell types. The CPHi population was actually a diverse mix, primarily made up of:
- Cycling TEX: Actively dividing cells, indicating a robust immune response.
- Terminally Exhausted TEX: Cells that have been fighting for a while and are less active.
- Cytotoxic-like TEX: Cells specialized in killing target cells, including cancer cells.
- Resident Memory-like TEX: Cells that stick around in the tissue, providing long-term surveillance.
- Glycolytic TEX: Cells with enhanced glucose metabolism, which often fuels immune activity.
So, what does this all mean? Our findings suggest that CPHi TILs are a strong indicator of a good response to treatment in melanoma patients. However, these CPHi TILs aren’t a uniform group; they’re a heterogeneous team with diverse players potentially contributing to anti-tumor immunity after checkpoint blockade. This highlights the complexity of the immune response and underscores the need for further research to fully understand how these different subpopulations work together to fight cancer. This knowledge will pave the way for developing even more effective, personalized cancer immunotherapies.
