Imagine a lock and key. PD-1 pathway inhibitors, a revolutionary cancer therapy, are like a key designed to unlock the body’s own immune system to fight cancer. However, this key doesn’t work for everyone, and scientists are working hard to understand why. They’re searching for specific “biomarkers,” like clues within the tumor, that can predict who will benefit from this treatment and who won’t.
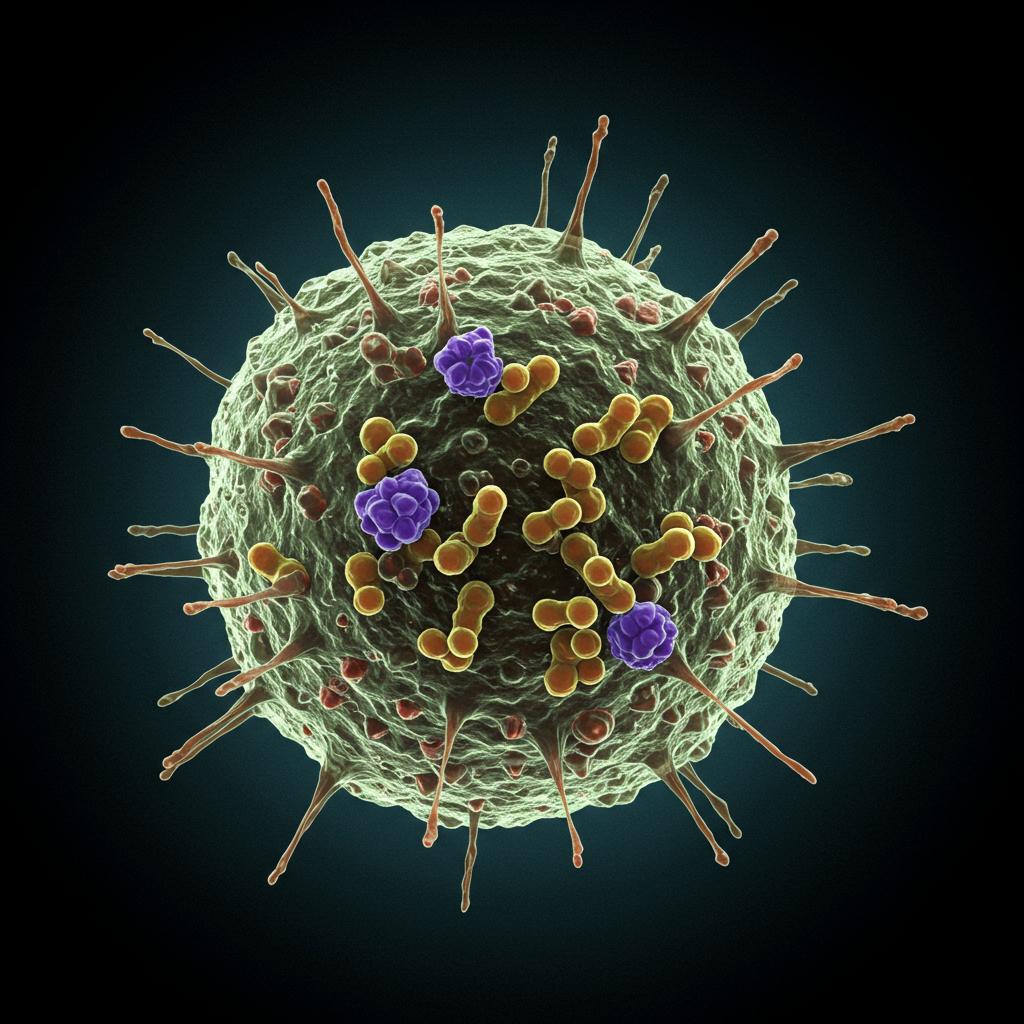
One area of focus is a type of immune cell called CD8+ tumor-infiltrating lymphocytes (TILs). Think of these as the body’s special forces soldiers, infiltrating the tumor to destroy it. While it’s known that higher numbers of CD8+ TILs are generally good, it’s like having a large army without knowing which soldiers are the most effective fighters. Researchers are trying to identify the specific types of CD8+ TILs that pack the biggest punch against cancer.
Early research highlighted “progenitor-like exhausted” CD8+ T cells (TPEX). These are like the fresh recruits, full of potential and ready to multiply and fight when activated by PD-1 inhibitors. However, it turns out that during treatment, these TPEX cells change into other types of exhausted T cells (TEX), and some of these evolved cells are actually the key players in eliminating the tumor. This makes it tricky to pinpoint the most important TILs just before treatment begins.
Our study looked at advanced melanoma patients and found an exciting correlation. Patients with a high percentage (20% or more) of CD8+ TILs that express both PD-1 and CTLA-4 (we call these CPHi TILs) responded better to PD-1 inhibitor therapy and lived longer. Think of these CPHi TILs as having double the identification markers, making them easier to spot.
But there’s more to the story. When we analyzed these CPHi TILs in detail using advanced techniques like RNA sequencing, we discovered that they’re not just one type of cell. It’s like discovering that our “special forces” team is actually made up of different specialist units. While some TPEX cells are present within the CPHi group, they are outnumbered by other TEX cell types, including:
- Cycling TEX: These are actively dividing and multiplying, suggesting ongoing anti-tumor activity.
- Terminally Exhausted TEX: These cells might sound ineffective, but they could still play a supporting role in the immune response.
- Cytotoxic-like TEX: These are the heavy hitters, directly killing cancer cells.
- Resident Memory-like TEX: These cells stick around in the tumor environment, providing long-lasting protection.
- A subset with high glycolytic activity: These cells are fueled by sugar and may have enhanced energy production for sustained fighting power.
So, while having high levels of CPHi TILs is a good sign for melanoma patients considering PD-1 inhibitors, it’s not just about the sheer number of these cells. The diversity within the CPHi population, this mix of different specialist units, likely contributes to a more effective anti-tumor response. This research helps us better understand which “soldiers” are crucial in the fight against melanoma, paving the way for more personalized and effective cancer therapies.
